Discussing spinal surgery in cerebral palsy and funding the costs of SDR and curvature surgery

By Abigail Ringer and Tim Theologis (Consultant Orthopaedic Surgeon and Associate Professor at the University of Oxford).
Surgical treatment of the spine, whether that is to treat curvature of the spine or to carry out selective dorsal rhizotomy, has become a mainstay of treatment for children and young people with cerebral palsy. As a parent or carer of a child with cerebral palsy, it is not always an easy decision to proceed to surgery. Both the likely benefits need be considered against the known risks of surgery. In addition, for some, the cost of surgery will hang heavily in the balance.
At RWK Goodman we represent families affected by cerebral palsy, securing compensation that will meet the cost of a child’s care, treatment and equipment needs throughout their life. In calculating how much money a child will need, we always consider their individual likelihood of requiring spinal surgery both now and in the future. In doing so, we rely heavily on the advice of experts such as Mr Theologis, Consultant Orthopaedic Surgeon and Associate Professor at the University of Oxford, who has kindly contributed his experience to this article.
The surgical treatment of curvature of the spine
What is curvature of the spine?
Curvature of the spine, or scoliosis, occurs when the spine develops a sideways curvature. Curvature of the spine is common in people with cerebral palsy who are unable to walk independently or with support. Poor posture due to increased stiffness of the muscles and muscle weakness can contribute to a lack of support of the spine. The reported incidence of scoliosis among people with cerebral palsy varies between different studies but overall, it seems to be that around 20-25% of those affected by cerebral palsy are also affected by curvature of the spine, albeit this percentage increases as the severity of cerebral palsy increases[1].
When does spinal surgery for curvature of the spine become necessary?
Severe scoliosis can be painful and reduce quality of life. It can also make breathing more difficult and make sitting and transfers more uncomfortable. Therefore, the overall goal in managing spinal deformity is to maintain, or ideally improve, functional ability and quality of life.
Treatment of curvature of the spine generally starts with conservative measures such as adaptive seating, progressing to spinal orthoses and, finally, surgical treatment. A study in Oxford found that by adapting seating, with the inclusion of pads at the side of the body, a significant improvement to the shape of the spine can be achieved[2]. A spinal orthosis acts in a similar but more consistent way, providing an external support aid to the spine. Some children do not tolerate the spinal orthosis. In particular, the spinal orthosis is poorly tolerated by children who have breathing difficulties.
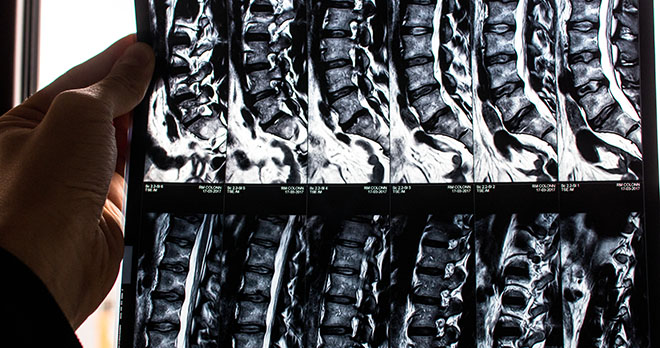
When more conservative options for the treatment of scoliosis have been exhausted, surgical treatment of the spine will be considered. Surgical treatment for scoliosis (spinal fusion) involves inserting metal rods to support the spine and bone graft that leads to fusion of the vertebrae, the bony blocks of the spine, so that they form a single bone. Once bony fusion is completed (usually within 6 months) the rods become redundant but are not routinely removed unless they cause problems.
What are the risks and benefits of spinal surgery?
One way of measuring quality of life is by reference to the Caregiver Priorities and Child Health Index of Life with Disabilities (CPCHILD) questionnaire[3]. The questionnaire asks parents and carers to consider the level of difficulty a child has in performing certain tasks over the course of the previous two weeks such as eating and drinking, dressing, toileting and getting in and out of car; and the level of pain or discomfort experienced during those tasks. The questionnaire also explores mood, communication skills and overall quality of life.
A study carried out in Boston, USA, compared CPCHILD questionnaire scores for children with cerebral palsy both before and after spinal surgery[4]. The study found that at one year after surgery, the overall scores had increased, reflecting a positive increase in the parent’s or caregiver’s perception of the child’s quality of life but that at two years after surgery, the CPCHILD scores were back at the baseline, reflecting no overall improvement. However, another study from British Columbia, Canada, found that parents and caregivers reported improvements on the CPCHILD questionnaire at one, two and five years postoperatively[5].
A decision to provide surgical treatment should be given thorough consideration because of the risks involved. The risks of spinal fusion surgery include postoperative chest infection; blood loss during the operation; and wound infection. However, for those with cerebral palsy, the risks of each of these can be higher due to weakness in the chest muscles and swallowing difficulties; clotting abnormalities from medication; and the increased potential for infection caused by being incontinent[6]. These risks and complications should be balanced against the risk of severe scoliosis compromising cardiopulmonary function and quality of life.
How much does spinal surgery cost?
When spinal surgery for curvature of the spine becomes necessary, many people will choose to have this under the care of the NHS. For others, treatment in the private sector is an option. The average cost of such treatment in the private sector would be in the range of £42,000 – £48,000. However, this can vary considerably between different Institutions .
- [1] Incidence of scoliosis in cerebral palsy – PMC (nih.gov)
- [2] Management of scoliosis with special seating for the non-ambulant spastic cerebral palsy population–a biomechanical study – PubMed (nih.gov)
- [3] PSCORE | CPCHILD (sickkids.ca)
- [4] Health-Related Quality of Life and Care Giver Burden Following Spinal Fusion in Children With Cerebral Palsy – PubMed (nih.gov)
- [5] Assessing the Risk-Benefit Ratio of Scoliosis Surgery in Cerebral Palsy: Surgery Is Worth It – PubMed (nih.gov)
- [6] Development and treatment of spinal deformity in patients with cerebral palsy – PMC (nih.gov)
Selective Dorsal Rhizotomy Surgery
What is Selective Dorsal Rhizotomy Surgery?
Selective Dorsal Rhizotomy (SDR) surgery is another surgical procedure to the spine. It is used to reduce the spasticity (stiffness) of muscles in the lower limbs of children with spastic cerebral palsy and involves partially cutting selected sensory nerves inside the spine of the lower back. Cutting these nerves reduces the abnormal signals that pass between the brain and the legs in those who experience spasticity of the lower limbs. Surgery is followed by intensive physiotherapy.
When does Selective Dorsal Rhizotomy surgery become necessary?
There are several treatment options available for people affected by spastic cerebral palsy which aim to reduce the stiffness of muscles and improve function. It is important to distinguish between treatments that address the primary problem (spasticity) and those that address the secondary problem of muscle stiffness. These are shown in the table below:
| Primary Spasticity | Secondary Muscle Problems |
| Oral medications for spasticity and/or dystonia (Neurology) | Physiotherapy |
| Selective Dorsal Rhizotomy (Neurosurgery) | Casts |
| Intrathecal Baclofen (Neurosurgery) | Orthotics (splints and braces) |
| Botulinum toxin injections | Orthopaedic Surgery |
Surgical treatment for spasticity in the form of Selective Dorsal Rhizotomy tends to be considered only in limited circumstances. It is important to understand that the procedure is irreversible and there are associated complications.
NHS England has produced a detailed policy of when Selective Dorsal Rhizotomy should be made available on the NHS for the treatment of spasticity in cerebral palsy[1]. The policy provides that SDR surgery on the NHS is available to children between the ages of 3 and 9 who meet the following criteria:
- a) A diagnosis of cerebral palsy with spasticity mainly affecting the legs;
- b) The child has dynamic spasticity in lower limbs affecting function and mobility and no dystonia;
- c) The MRI brain scan shows typical cerebral palsy changes and no damage to key areas of brain controlling posture and coordination;
- d) The child functions at GMFCS level II or III[2];
- e) There is no evidence of genetic or neurological progressive illness;
- f) The child has mild to moderate lower limb weakness with ability to maintain antigravity postures; and
- g) The child has no significant scoliosis or hip dislocation.
How much does SDR spinal surgery cost?
Many people affected by spasticity of the lower limbs do not meet the criteria set down by NHS England and look to explore alternative funding options. According to the Tree of Hope website[3], costs for SDR surgery range from around £20,000 to £30,000 and treatment after the procedure can also be expensive. Physiotherapy, on the lower end of the scale, can cost around £4,000 per year, but depending on how long therapy is required, costs could rise to around £13,000.
Some treatment centres (such as the spasticity centre in Leeds) offer a “self funding” programme to UK NHS patients who are 10 years old and over but who otherwise meet the criteria for surgery. These children receive surgery and 3 weeks of post-operative physiotherapy at cost[4]. Other centres provide similar programmes.
Not all families can afford SDR surgery when NHS funding is unavailable and many turn to online funding platforms such as Crowdfunder and Go Fund Me. Cauldwell Children’s Charity has been supporting children to access SDR surgery and post-operative therapy since 2012 and may offer both a financial contribution to the cost or provide practical fundraising support[5].
Raising a child with cerebral palsy can be expensive and the potential cost of spinal surgery is only a small part of the additional cost of life with a differently-abled child. At RWK Goodman, we work with experts in orthopaedic surgery; neurology; physiotherapy; occupational therapy; speech and language therapy and assistive technology and consider the current and future needs of a child on an individual basis. We pride ourselves on going the extra mile so that every additional need of a child is included in their claim for compensation, ensuring that the funds are available to meet those needs for life.
- [1] NHS England, Clinical Commissioning Policy: Selective Dorsal Rhizotomy (SDR) for the treatment of spasticity in Cerebral Palsy (children aged 3-9 years). NHS Reference 170063P March 2019 and updated July 2019.
- [2] The Gross Motor Function Classification System (GMFCS) – is a standardised 5-level classification system that describes the gross motor function of children and young people with cerebral palsy on the basis of their self-initiated movement with particular emphasis on sitting, walking, and wheeled mobility. Distinctions between levels are based on functional abilities, the need for assistive technology, including hand-held mobility devices (walkers, crutches, or canes) or wheeled mobility, and to a much lesser extent, quality of movement.
- [3] Selective Dorsal Rhizotomy (SDR) for Cerebral Palsy – Tree of Hope
- [4] www.LeedsNeurosurgery.com | Patient Information | Selective Doral Rhizotomy
- [5] Selective Dorsal Rhizotomy Financial Support – Caudwell Children

It is with great pride in our personal injury and clinical negligence teams, and the experts and charities that they work with, that we present this edition of Team Around the Client magazine focusing on spinal medical and legal issues.
If you have questions about making a claim for cerebral palsy, contact our enquiries team today.
Call now