Cerebral palsy - the condition, causes, and legal issues
Download our guide to cerebral palsy
Find out all you need to know about the condition, treatments, support available and more in our guide.
Our birth injury experts have collated a range of information for families affected by cerebral palsy in this comprehensive guide.
Cerebral palsy is a non-progressive condition – i.e. one that doesn’t get worse over time – that affects movement, co-ordination, balance and posture. It can, therefore, affect a person’s gross motor ability, such as crawling, standing, walking and running; and fine motor ability, such as grasping, dressing, eating and writing. It may also affect vision, communication, learning and behaviour.
Please browse the information below to find out more about the different types of cerebral palsy, what symptoms might be present, how it may have been caused, and when to seek legal advice.
Types of cerebral palsy
Each type of cerebral palsy will affect a person’s muscle control and movement in different ways, and many people with cerebral palsy will have a combination of types.
Cerebral palsy is also classified by its severity (mild, moderate or severe) and no two cases of cerebral palsy are the same.
Families and health professionals can use the Gross Motor Function Classification System (GMFS) to describe the abilities of children and young people with cerebral palsy. It categorises abilities into five levels that are used to decide on the most appropriate and effective treatment and therapies.
We describe the different types of cerebral palsy and the classification system in more detail below.
Spastic cerebral palsy occurs in more than 70% of all cases. Spasticity, a form of hypertonia, is a state of increased muscle tone or excessive muscle contraction affecting different areas of the body.
Spastic cerebral palsy is a neuromuscular (nerve and muscle) mobility impairment, caused by injury to the brain in the pyramidal tract. This type of injury is also referred to as upper motor neuron damage. It’s characterised by an often painful rigidity, tightness or ‘pull’ in the muscle that decreases its range of movement. The muscle(s) may often go into spasm.
Along with limbs, the tongue may be affected. This may affect speech, eating, breathing and swallowing.
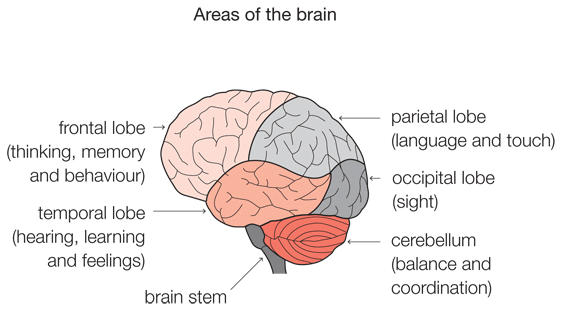
Ataxic cerebral palsy features in 5-10 per cent of people with cerebral palsy. It is caused by damage to the cerebellum – the region of the brain that coordinates muscle movement. This causes an interruption of muscle control resulting in a lack of balance, coordination and depth perception.
The movements of someone with ataxic cerebral palsy may therefore seem jerky or shaky. The person may also experience tremors/shaking in their muscles when carrying out specific actions, such as writing.
Ataxic cerebral palsy can affect limbs, eye movements and the muscles involved in swallowing. People with the condition may also walk with a wide gait.
Ataxic cerebral palsy can cause hypotonia (reduced muscle tone or floppy/loose muscles) which further impedes movement. Young babies with ataxic cerebral palsy are often noted to be ‘floppy’.
Dyskinetic cerebral palsy includes both athetoid cerebral palsy and dystonic cerebral palsy, affecting around 15% of people with the condition.
A person with dyskinetic cerebral palsy will experience variable movements outside of their control, made worse by an attempt to move. The condition is caused by damage to the basal ganglia and thalamus, the area of the brain responsible for regulating voluntary movements.
Different forms of dyskinesia result from damage to different structures within the basal ganglia (athetoid cerebral palsy, dystonic cerebral palsy and choreoathetoid cerebral palsy).
Athetoid cerebral palsy is a type of dyskinetic cerebral palsy characterised by involuntary slow, continuous writhing movements, usually affecting the hands, feet, arms or legs and sometimes the whole body. Facial muscles, lip and tongue movements can also be affected, and therefore speech, eating and drinking can be difficult. Movements are made worse by attempts to move and increase under emotional or physical stress. They are present even when the body is at rest but disappear when the person is asleep.
Unlike with spastic or ataxic cerebral palsy, people with athetoid cerebral palsy will experience fluctuations in muscle tone, i.e. they have both hypotonia (reduced muscle tone) and hypertonia (increased muscle tone). This can make it difficult to maintain a position like sitting or standing.
Choreoathetoid cerebral palsy is when athetoid cerebral palsy occurs with chorea. Chorea is characterised by involuntary movements that are irregular, unpredictable and brief. It affects various parts of the body and also speech and swallowing.
Dystonic cerebral palsy is a type of dyskinitic cerebral palsy resulting in involuntary muscle contractions, characterised by slow twisting or repetitive movements and awkward, sustained postures. These contractions are triggered by an attempt to move, and may become increasingly frequent and painful when the person is tired or stressed.
Dystonic cerebral palsy chiefly affects trunk muscles (resulting in a fixed, twisted posture), but can also affect a combination of limbs and trunk muscles. This is known as generalised dystonia. Speech and swallowing can be affected.
Focal dystonia is when the condition affects only one part of the body, such as a person’s foot, and is triggered by a specific task or movement.
Cerebral palsy can affect different parts of the body. The terms diplegic, hemiplegic and quadriplegic are used to describe the number of limbs affected:
- Diplegic cerebral palsy affects both legs. The arms may be affected to a lesser extent
- Hemiplegic cerebral palsy affects just one side of the body (one arm and one leg)
- Quadriplegic cerebral palsy affects both arms and legs and the muscles of the trunk, face and mouth can also be affected.
Cerebral palsy may be described as hypertonic or hypotonic:
- Hypertonia results in stiff and rigid muscles with excessive tone (as characterised in spastic cerebral palsy)
- Hypotonia results in diminished muscle tone or loose/floppy muscles (as characterised in ataxic cerebral palsy).
People with athetoid cerebral palsy experience both hypertonia and hypotonia.
The Gross Motor Function Classification System
The Gross Motor Function Classification System (GMFCS) is a universal classification system that helps families and health professionals to:
- Categorise the severity of a child’s cerebral palsy
- Provide a clear description of a child’s current motor function (e.g. head control and their ability to walk, sit, run, jump and use wheeled, hand-held, motorised or manual mobility aids)
- Decide on the most appropriate treatment, surgery, therapies and mobility aids.
The tool focuses on what the child can accomplish, categorising their motor function abilities into five different levels.
Children at level 1 will be able to walk without restrictions and their symptoms may be described as mild. Children at level 5 are restricted in their ability and generally transported in a manual wheelchair. Their symptoms would be described as severe. Children are graded upon what they normally can do at home, school and in the community, rather than their best attempts.
There are five age bands (under 2, 2-4 years, 4-6 years, 6-12 years, and 12-18 years). By age 5, a child will be unlikely to improve their GMFCS level.
Health professionals will routinely grade your child using the GMFCS, but you can also complete a family report questionnaire, classifying your own child’s motor abilities.
The GMFCS can be downloaded for personal use at no cost from the CanChild website (based in Canada).
Diagnosing cerebral palsy
Cerebral palsy is caused by damage to the brain or abnormal development of a baby’s brain during its development, delivery or post-natal period.
Despite the condition being present at birth, cerebral palsy can be difficult to diagnose early. In fact, doctors may wait until a child is 24 to 36 months old to make an official diagnosis. This is because early symptoms of cerebral palsy can be confused with other conditions that grow worse over time or are temporary.
When a baby is born, doctors will check a baby’s voluntary movements and muscle tone. They will carry out clinical observations, such as a general movement assessments in a child under four months old. This provides one of the most accurate ways of identifying motor function problems early on. But this assessment cannot predict the severity of the condition.
Health visitors and doctors will also look for signs that a baby is meeting all of its developmental milestones, such as grasping, turning its head, rolling over and sitting up etc., but it is often the parents who first notice significant delays. If doctors are concerned, this will prompt further investigations. See the list of developmental milestones below.
If cerebral palsy is suspected, further diagnostic tests such as neuroimaging with CT (computerised tomography) or MRI (magnetic resonance imaging) will help to confirm it and identify the damage to the brain. The area of damage will indicate what type of cerebral palsy a child has, but it may be difficult to assess the full impact of the condition until the child is 24 to 36 months old.
In babies, signs of possible cerebral palsy visible from birth include:
- Tight or floppy muscle tone
- Unusual postures
- A preference for using one side of the body
- Feeding or swallowing difficulties
- Developmental delays
In toddlers, investigations will start if your child is not walking by 12-18 months and not speaking simple sentences by 24 months.
Developmental delays that can indicate cerebral palsy
A baby’s normal development is charted by its ability to do certain things within a certain age bracket, such as sit up, grab toys, smile, roll over and walk. These abilities are referred to as developmental milestones.
If your baby is slow to meet these development milestones it may be that nothing is wrong. If your doctor or health visitor is concerned though, it could trigger a series of investigations to establish the cause of the delay.
Examples of milestones that indicate normal development and gross motor skills include:
At the end of two months (eight weeks) old:
- Beginning to hold head up
- Attempts to push up when lying on tummy
- Smoother arm and leg movements.
At the end of four months (16 weeks) old:
- Attempts or can roll over from tummy to back
- Holds a toy or attempts to grab hanging toys
- Pushes up when lying on tummy
- Can bring hand to mouth.
At the end of six months old:
- Begins to sit without support
- Can roll over
- Can support weight on legs when standing
- Rocks back and forth in an attempt to crawl.
In toddlers, investigations will start if your child is not walking by 12-18 months and not speaking simple sentences by 24 months.
If you are concerned that your baby is not meeting its developmental milestones, contact your health visitor or doctor. You can find out more about developmental milestones at the NHS website (Birth-to-Five Development Timeline).
The symptoms of cerebral palsy
Symptoms will vary from person to person, depending on how your child’s brain was damaged. The condition will therefore affect different people in lots of different ways depending on the type of cerebral palsy and its severity. Symptoms can be uncomfortable and often painful.
People with cerebral palsy may also experience a wide range of associated physical and learning difficulties. These include:
- Hip and spine problems (hip dislocation, curvature of the spine)
- Fits or seizures (epilepsy)
- Vision and/or hearing impairment
- Bladder and bowel problems
- Communication difficulties (speaking, comprehending)
- Drooling and swallowing difficulties
- Specific learning difficulties
- Behaviour difficulties.
We examine the physical symptoms and associated difficulties experienced by people with cerebral palsy in more detail below.
The muscle-related disabilities caused by cerebral palsy will vary according to the type of cerebral palsy a person has, the number of limbs/muscles affected, and the condition’s severity.
General disabilities can include:
- Impaired movement and ability to control the affected area of the body, such as arms, legs, hands, feet, trunk, face, fingers, tongue
- Impaired gross motor skills such as walking, running, jumping and transferring positions
- Impaired fine motor skills such as eating, writing, grasping
- Painful muscle spasms and contractions.
In people with spastic cerebral palsy, and depending on the limbs affected, disabilities can include:
- Extremely stiff muscles (hypertonia) making movement jerky, shaky or impossible
- Difficulty standing, sitting, moving to another position, walking and running
- Bent elbows, wrists and fingers
- Flexion at the hip and knee (bending or a bent condition)
- Scissoring of the thighs (also referred to as adduction)
- Equinovarus foot, where tight calf muscles raise the heel and cause the foot to point down and inwards
- Impaired speech, eating and drinking
- Loose or floppy muscles caused by decreased muscle tone (hypotonia)
- Tremors caused by contracting muscles.
The effects of spasticity on the muscles can cause associated problems such as:
- Muscle pain
- Atrophy of muscles (deterioration/wasting)
- Fibrosis
- Contracture of the joints
- Bone deformities.
In people with ataxic cerebral palsy, where balance and depth perception is affected, muscle-related disabilities include:
- Uncoordinated, shaky movements
- Lack of balance and clumsiness
- Tremors in the arms and hands particularly when performing precise movements
- Inaccurate movements / overshooting targets
- Instability when walking (falling over)
- Speech and swallowing difficulties
- Slow eye movements.
In people with dyskinetic cerebral palsy, which includes athetoid, choreoathetoid and dystonic cerebral palsy, muscle-related disabilities include:
- Involuntary movement outside of a person’s control, triggered by an attempt to move
- Drooling and grimacing if the tongue and facial muscles are affected
- Impaired speech, eating and drinking.
Symptoms and pain are often made worse by physical and emotional stress.
In athetoid cerebral palsy, muscle-related disabilities include:
- Difficulty maintaining a position such as sitting or standing due to fluctuations in muscle tone (a person experiences both hypertonia and hypotonia)
- Slow, continuous writhing movements
- Random or repetitive movements outside of a person’s control
- Difficulty holding objects
In dystonic cerebral palsy, muscle-related disabilities include:
- Slow, twisting repetitive movements
- Limbs forced into awkward/uncomfortable and sustained positions.
In choreoathetoid cerebral palsy, muscle related disabilities include:
- Unpredictable and irregular involuntary movement combined with the muscle-related disabilities associated with athetoid cerebral palsy
- Movements that range from clumsy to violent, depending on the condition’s severity.
Around a third of children with cerebral palsy will also suffer from epilepsy, a condition associated with damage to the brain that causes seizures or fits. Fits can be severe, causing someone to lose consciousness, shake or enter into a trance-like state where no loss of consciousness is felt.
Cells (neurons) in the brain conduct electrical signals and communicate with each other using chemical messengers. Seizures are caused by abnormal bursts of neurons (cells) firing off electrical impulses.
Epilepsy cannot be cured but controlled with effective anti-epileptic drugs. Surgery may be recommended in severe cases.
People with epilepsy may need to adapt their lifestyle to manage their condition. They should seek advice before getting pregnant and about driving and contraception.
As well as affecting people’s manual ability, balance and posture, cerebral palsy can affect a person’s cognitive ability, which is their ability to understand and process information and the world around them.
That’s not to say that everyone with cerebral palsy will experience learning difficulties. Some people who are severely physically impaired will have average and above average intelligence and understanding.
Impaired cognitive ability in people with cerebral palsy is usually a result of their brain injury, and the extent of impairment will depend on where in the brain the injury occurred and the level of damage.
Damage to the brain could result in specific learning difficulties, such as difficulty spelling. In these cases overall intelligence is not impaired. When damage to the brain affects overall intellectual functioning and language development, it is referred to as a learning disability or a severe learning disability.
One way of measuring a person’s cognitive ability is an IQ test. IQ stands for intelligence quotient, and an IQ assessment is a standardised way of measuring a person’s ability to think and reason compared with other people the same age. A score of 100 is ‘average intelligence’ and usually someone with impaired cognitive ability will score 70 or below.
Many more people with cerebral palsy will experience a range of learning difficulties simply as a result of their reduced physical abilities and the discomfort directly associated with their condition. Symptoms of cerebral palsy can affect sleep, concentration, coordination and wellbeing, and therefore a person’s ability to learn.
Aids and support can help people living with cerebral palsy to overcome their difficulties.
Learning difficulties in people with cerebral palsy can be mild, moderate or severe and may only be related to a specific area of learning.
If a child with cerebral palsy has difficulty with a specific skill, such as spelling or arithmetic, but their overall intelligence is not affected, this is called a specific learning difficulty.
Where damage to the brain is extensive and language development and overall intellectual function is affected, this is referred to as a severe learning disability.
It is important to remember that many people with severe physical disabilities will have normal and above normal intelligence.
Learning difficulties/disabilities can include:
- Short attention spans
- Difficulty organising and sequencing information
- Language difficulties
- Difficulty understanding concepts
- Difficulty remembering information
- Impaired decision-making.
Signs that a baby or child has a cognitive impairment can include:
- Delayed language development
- Difficulty in interacting/socialising with others
- Difficulties remembering information
- Angry outbursts
- Hearing and/or visual impairments.
Children with cerebral palsy who have learning disabilities may require special educational provision to be made for them so that they can reach their full potential in skills such as reading, writing, numeracy and comprehension. An assessment, provided by your local authority and your NHS care team, will identify any special educational needs.
Challenging behaviour or behavioural problems can be evident in all children and young people with cerebral palsy, regardless of the severity of the condition and their intelligence. It is more common in people with associated learning difficulties, such as impaired reasoning and communication difficulties.
Behavioural problems can include:
- Self-injury, including head banging, grinding teeth, scratching and eating inedible items
- Aggression towards others, including hitting, biting, screaming and verbal abuse
- General anti-social behaviour, including damage to belongings or property, stealing, inappropriate sexual behaviour and tantrums.
Less worrying behaviour exhibited by people with cerebral palsy may include rocking, repetitive speech and repetitive movements.
Ensuring a rich, stimulating environment and a means of effective communication is the first step to improving challenging behaviour. Professionals can also assess your child’s behaviour – and the factors influencing it – and advise on appropriate approaches and therapies to help.
We communicate with others using gesture and speech and good communication is vital to healthy development. It’s the way that we get to know one another, express thoughts and emotions and develop independence.
Unfortunately, 6 out of 10 children with cerebral palsy will have difficulty with speech, language and communication. Children with athetoid cerebral palsy are more likely to experience these difficulties.
Communication difficulties in people with cerebral palsy can be caused by:
- Reduced ability to control muscles in the face, respiratory system, tongue, vocal chords and eyes
- Reduced ability to control body language/posture
- Hearing impairments
- Visual impairments
- Associated learning difficulties
All of these problems can affect a person’s ability to communicate effectively.
Specific communication difficulties may include:
- Reduced ability to produce sounds or clear speech because a person cannot control or coordinate the muscles surrounding the mouth, tongue and/or vocal chords
- Coordinating breath to support speech
- Controlling body movements to enable clear speech
- An inability to produce sounds
- An inability to speak
- Reduced ability to express thoughts and emotions through speech, hands, eye contact and body language
- Reduced ability to write, type and indicate.
There are a variety of methods, technological aids, learning strategies and therapies available to help children, young people and adults with cerebral palsy to communicate effectively, even if their condition and communication difficulties are severe.
Good communication between you and your child is important, so seek advice as early as possible from a speech and language therapist, occupational therapist or physiotherapist.
What causes cerebral palsy?
When you talk to your doctor, paediatrician or specialist legal team about the possible causes of cerebral palsy, they may use complex terms and explanations.
Below we provide more detail about the causes of cerebral palsy and of brain injury, explain the medical terms often used, as well as when negligence may have occurred:
At all stages of life, the brain has enormous energy demands. Most of the energy is produced from a chemical reaction involving glucose and oxygen. Brain cells have poor energy storage facilities and as a result, the brain depends on a second-by-second supply of glucose and oxygen.
Oxygen is transported to the brain via blood circulating around the body. A drop in blood oxygen (hypoxia); and/or a disruption in blood flow (ischaemia) can result in energy deprivation.
Hypoxic-ischaemia describes an insult (injury) caused by a combination of the above.
When the brain is deprived of energy, the result is brain cell injury and brain cell death. The pattern of brain injury in hypoxic-ischaemia will depend on the severity and duration of the insult. In fetuses and babies, the pattern of brain injury will also depend on the maturity of the brain.
Perinatal refers to the short period before, during and after birth, and this is a risky time for suffering brain damage as a result of hypoxic-ischaemia. For example, if the umbilical cord is compressed during birth, it could disrupt blood flow to the baby’s brain. Or a difficult delivery may put too much strain on the baby’s cardiovascular system.
The pattern of brain injury will depend upon the severity and duration of the disruption, and on the maturity of the brain.
Acute near total hypoxic-ischaemia describes a situation whereby the energy deprivation is sudden and severe. In babies born at term, the areas of the brain most affected by this type of injury are the deep structures of the brain including the basal ganglia and thalamus.
The reason that this area of the brain is vulnerable to energy deprivation is because at this stage of a baby’s life, the brain cells of these deep structures have the highest energy demands in the brain.
The basal ganglia, thalamus and brain stem are involved with the coordination of movement. Children with this pattern of injury are likely to be severely disabled with movement disorders and in particular, athetoid cerebral palsy.
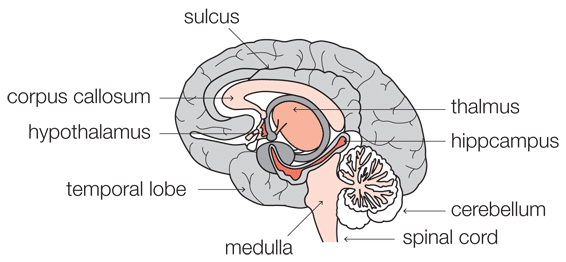
Chronic partial hypoxic-ischaemia happens when the energy deprivation is prolonged and only partial in severity. The different arteries of the brain supply blood to different territories of the brain. In mature infants, the brain cells within the border zones between these territories are the most vulnerable to this type of injury, and therefore chronic partial hypoxic-ischaemia results in damage to the outer reaches of the brain or the cortex.
Periventricular leukomalacia (PVL) is a form of brain damage affecting the area of the brain either side of two reservoir-like chambers known as the lateral ventricles. It is also known as white matter damage. In premature infants, this area of the brain is particularly vulnerable to the effects of both energy deprivation and infection, because the cells in this part of the brain have not yet developed their main defence mechanisms.
In premature infants, PVL is a pattern of injury seen in both acute near total hypoxic-ischaemia and chronic partial hypoxic-ischaemia.
Children who suffer from PVL may experience a wide range of problems depending on the severity of the injury. While some children may experience only minor disabilities in movement, a more severe injury may result in cerebral palsy and/or epilepsy.
Chorioamnionitis arises when the membranes and amniotic fluid surrounding the fetus become infected. This can arise when bacteria or other infective organisms travel from the vagina up in to the uterus, causing infection within the uterus and subsequent infection of the fetus.
Normally the fetus is protected from infection by a plug of mucus that sits in the cervix and by the membranes that surround it, but once rupture of membranes has occurred, the fetus is much more vulnerable to infection.
Occasionally the infective organisms reach the uterus by travelling across the placenta, or they can enter the uterus during invasive procedures such as amniocentesis.
Once the fetus becomes infected, the bacteria can travel to the brain where it can cause an infection of the membranes surrounding the brain, otherwise known as meningitis (see below).
Group B Streptococcus (GBS) is a type of bacteria that can cause chorioamnionitis. GBS is part of the normal flora of the vagina so most mothers who carry GBS are not aware that they carry it.
Like other types of bacteria, GBS can travel into the uterus from the vagina to cause chorioamnionitis and subsequent infection of the fetus. Alternatively babies can become infected with GBS during delivery.
Once the fetus or baby becomes infected with GBS the bacteria can travel to the brain where it can cause an infection of the membranes surrounding the brain, otherwise known as meningitis (see below).
Meningitis is an infection of the meninges, the three layers of membrane that envelop the brain and the spinal cord.
The outermost layer lies under the skull. It is a thick membrane known as the dura mater, which literally means ‘tough mother’. The next layer is the arachnoid mater, which looks a bit like a spider’s web, hence the reference to ‘arachnoid’. The final layer, which lies over the brain itself, is the pia mater, which can be translated as ‘gentle mother’. Between the arachnoid mater and the pia mater is the arachnoid space. The arachnoid space is full of cerebrospinal fluid (CSF), a watery substance that circulates around the brain.
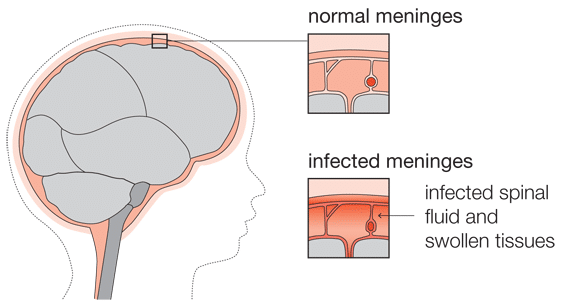
The lining of blood vessels within the brain is thicker than elsewhere in the body, providing a protective barrier (the blood-brain-barrier) between the circulating blood and the brain itself. It allows essential nutrients to pass through the lining but blocks harmful organisms.
Various types of viruses and bacteria can infect the meninges. In newborn babies, meningitis is commonly caused by streptococcus group B and E coli bacteria.
The bacteria may spread to the meninges from an adjacent infected area, or via the blood stream, penetrating the brain where the blood-brain-barrier is weak.
In some situations, for example where there is a congenital abnormality or where there has been a surgical procedure to the brain, the bacteria can reach the meninges by direct contact between the meninges and the outside world.
Once bacteria enters the cerebrospinal fluid, it can spread and multiply quickly.
Brain damage in bacterial meningitis is caused by the toxins released from the bacteria and also by the body’s own response to infection.
Toxins released from the bacteria damage brain cells but also cause damage to blood vessels, leading to a lack of blood (ischaemia) and energy reaching the brain cells.
When the bacteria are detected by the immune system, the immune system releases chemical messengers called cytokines, which in turn attract white blood cells. The white blood cells ingest the bacteria, but the process of ingesting the bacteria leads to the release of toxins that can damage both brain cells and blood vessels.
Although the immune system serves to protect the brain and body, the system starts a destructive cascade that can cause as much damage to the brain as the bacteria it aims to eliminate.
Children who have suffered from meningitis may experience different types of brain damage, depending on which areas of the brain were affected. This can result in cerebral palsy, epilepsy, vision and hearing loss and intellectual difficulties.
At all stages of life, the brain has enormous energy demands. Most of the energy is produced from a chemical reaction involving glucose (sugar) and oxygen.
Brain cells have poor energy storage and as a result, the brain depends on a second-by-second supply of glucose and oxygen. Oxygen and glucose are transported to the brain via blood circulating around the body. A drop in blood oxygen (hypoxia); a drop in blood glucose (hypoglycaemia); and/or a disruption in blood flow (ischaemia) can all result in energy deprivation.
Under normal conditions, the body carefully maintains levels of blood glucose. When blood glucose levels rise, glucose is turned into glycogen that can be stored in the body. This reduces the amount of glucose in the blood and blood glucose levels are restored. Conversely, when blood glucose levels drop, glycogen is turned back into glucose, and blood glucose levels are maintained.
Hypoglycaemia is when levels of blood glucose are too low. Premature babies (and newborns) are particularly vulnerable to hypoglycaemia because they have deficient glycogen stores. Other causes of hypoglycaemia include a simple lack of blood glucose due to inadequate feeding or too much insulin. This causes poor regulation of blood glucose levels by turning too much glucose into glycogen.
When the brain is deprived of energy, the result is brain cell injury and brain cell death. The pattern of brain injury in hypoglycaemia will depend on the severity and duration of the insult. Babies who have suffered from hypoglycaemia may go on to suffer from developmental delay, epilepsy and cerebral palsy.
Microcephaly describes a head that is smaller than normal because the brain has not developed properly. Most cases of microcephaly have a genetic cause but microcephaly may be caused by brain injury as a result of hypoxic-ischaemia or infection.
Microcephaly is sometimes the first indication that a baby has suffered from an infection or a period of hypoxic-ischaemia (energy deprivation) affecting the brain.
The impact of microcephaly will depend upon the nature of the injury to the brain. Babies and children who have microcephaly may go on to suffer from developmental delay, epilepsy and cerebral palsy.
Intrauterine growth restriction (IUGR) refers to poor growth of a fetus while in the mother’s womb during pregnancy.
Fetuses require energy for development and growth. Most of the energy is produced from a chemical reaction involving glucose (sugar) and oxygen, delivered to the baby from the placenta via the umbilical vein.
A drop in blood oxygen (hypoxia); a drop in blood glucose (hypoglycaemia); and/or a disruption in blood flow (ischaemia) can all result in energy deprivation to the developing fetus and the rate of growth is reduced.
The causes can be many such as poor maternal nutrition or anaemia. Children who have suffered from IUGR may experience memory and learning difficulties.
An intraventricular haemorrhage occurs when blood escapes into the ventricles of the brain. The brain is surrounded by cerebrospinal fluid (CSF) that circulates around the brain and through reservoir like structures known as the ventricles.
Once blood escapes into the ventricles, blood clots may prevent the circulation of CSF around the brain. The ventricles may expand, causing damage to the surrounding brain tissue. The accumulation of fluid within the brain leads to a condition known as hydrocephalus. In the worst-case scenario, the build-up of CSF increases intra-cranial pressure to such an extent that the patient dies.
Perinatal intraventricular haemorrhage can occur at any time but usually develops a few hours after birth. Premature babies are most vulnerable to intraventricular haemorrhage because the developing brain still contains a thick layer of immature cells under the lining of the ventricles. This layer of cells is called the germinal matrix.
The germinal matrix is fragile and has an abundant blood supply. When it is damaged as a result of hypoxic ischaemia, infection or occasionally trauma, blood escapes into the ventricles of the brain.
Children who have suffered from intraventricular haemorrhage may experience developmental delay and cerebral palsy.
The terms ‘germinal matrix haemorrhage’ and ‘intraventricular haemorrhage’ are commonly interchangeable in premature babies.
Bilirubin is a product of the breakdown of red blood cells. When red blood cells are first broken down, the bilirubin that is produced is insoluble in water and is referred to as ‘unconjugated bilirubin’.
Unconjugated bilirubin then travels to the liver where it is converted into conjugated bilirubin that is soluble in water. This process enables it to be readily excreted from the body in faeces or in urine. The enzyme responsible for converting unconjugated bilirubin into conjugated bilirubin is called glucoronyl transferase.
Bilirubin can build up in the body when either too much of it is being formed (usually due to an increase in red blood cell breakdown) or because the body is having difficulty getting rid of it, e.g. there is a problem with the conversion of unconjugated bilirubin into the water-soluble conjugated bilirubin.
Kernicterus (bilirubin encephalopathy) is caused by the build-up of unconjugated bilirubin and can occur in newborn babies either as a result of a blood disorder leading to the breakdown of too many red blood cells, or because the liver cannot convert bilirubin to its water-soluble state. The latter is more common in premature babies who lack glucoronyl transferase, the enzyme required to conjugate bilirubin.
The unconjugated bilirubin is able to cross from the blood into the brain where it is able to bind to brain cell membranes and exert its toxic effects on the brain cell, resulting in cell death.
Bilirubin has a particular affinity for the deep areas of the brain responsible for voluntary movement and this is why a brain injury due to excess bilirubin can lead to cerebral palsy. Bilirubin-induced brain damage can also result in developmental delay and hearing problems.
Legal issues relating to cerebral palsy
There are many ways in which cerebral palsy can occur, as we have identified. Negligent treatment of each of these issues may mean that your child is entitled to compensation for their injury.
Find out more about the most common negligent causes of cerebral palsy below, as well as how life expectancy may factor into a claim:
If health providers fail to competently manage intrauterine growth restriction in pregnancy and this leads to a child developing cerebral palsy, you may be able to pursue a medical negligence claim.
Intrauterine growth restriction (IUGR) is when a baby’s growth slows down or stops during pregnancy. This might happen because of problems with the placenta, which is the organ responsible for supplying oxygen and nutrients to the fetus.
A baby suffering from growth restriction can suffer complications during pregnancy, labour and in the neonatal period. These complications include oxygen deprivation, low blood sugar and jaundice.
If these complications are not managed correctly, the baby could suffer permanent brain damage leading to cerebral palsy.
Concerns about growth restriction can be identified during pregnancy, usually during the regular measurements of the fundus (pregnancy bump) carried out by midwives at routine antenatal appointments.
If IUGR is diagnosed or suspected, then it should lead to more careful monitoring of the baby, including growth scans. A decision may be taken to deliver the baby early if there are concerns about the baby’s wellbeing.
Examples of negligence relating to the management of IUGR include:
- Failing to carry out regular and competent growth measurements during pregnancy
- Failing to identify concerns with growth measurements and/or refer for further investigations
- If IUGR is suspected, failing to carry out more careful monitoring of the baby’s wellbeing
- Failing to act on concerns as to the baby’s wellbeing and arrange early delivery by caesarean section or induction of labour.
If health providers fail to provide appropriate medical treatment for maternal infections and this leads to a child developing cerebral palsy, then there may be grounds to pursue a medical negligence claim.
Mothers can suffer from different infections during pregnancy, labour and delivery that can prove life threatening if passed on to their fetus or new baby. If these infections are not treated correctly, the baby could suffer severe brain damage. An example is group B streptococcus infection which can lead to meningitis and permanent brain damage.
Examples of negligence relating to the management of maternal infection include:
- Failing to deliver the child without delay when there are signs of fetal distress together with maternal infection
- Failing to treat maternal infection with appropriate antibiotics during labour and/or delivery
- Failing to provide appropriate antibiotics to the baby in the newborn period when there were signs of maternal infection during labour and/or delivery.
Midwives and obstetricians should carefully monitor the baby’s condition during labour and act on any signs of distress.
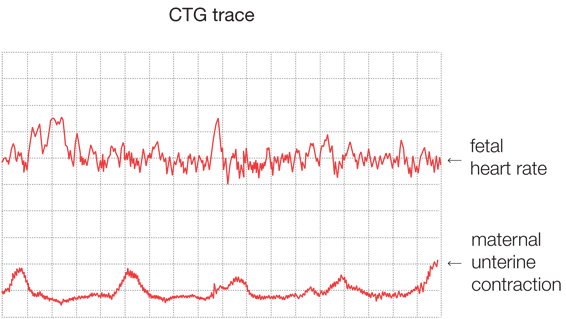
In low-risk labours, monitoring is carried out by intermittent auscultation, where the baby’s heart rate is listened to at regular intervals, but not continuously. If the midwives are concerned about the baby’s wellbeing, then further investigations and monitoring should be considered, including continuous monitoring of the baby’s heart rate by cardiotocography (CTG).
A CTG will produce a trace of both the fetal heart rate and maternal contractions. The features of the fetal heart (including rate, variability and accelerations/decelerations) are then categorised as normal/reassuring, non-reassuring or abnormal and, based on these features, the overall CTG trace is then graded as normal, suspicious or pathological. Where a trace is suspicious or pathological the midwife should call an obstetrician urgently.
Depending on the situation, the obstetrician may take a fetal blood sample (FBS) to check whether there is acidosis. This is an indication of oxygen deprivation.
If the sample is reassuring then labour will usually continue with close monitoring of the CTG trace and possible further blood samples.
If the sample is not reassuring, an emergency caesarean section should be considered. If the labour is too far advanced for a caesarean section to be practical, the obstetrician should assist the delivery (using forceps or ventouse) without delay.
Examples of negligence relating to the monitoring of fetal wellbeing during labour include:
- Failing to carry out appropriate monitoring, either at inappropriate intervals, or using only intermittent auscultation when continuous monitoring was indicated
- Failing to correctly interpret a CTG trace
- Failing to perform a fetal blood sample when indicated by the CTG trace
- Failing to act on a pathological CTG trace and/or non-reassuring fetal blood sample and delaying delivery when urgent delivery was indicated.
Either before or during labour, there may be signs that a vaginal delivery is inappropriate and that the mother should instead undergo a planned or emergency caesarean section. Risk factors include the position of the baby, lack of progress in labour and/or signs of fetal distress.
Examples of negligence in relation to the need for a caesarean section include:
- Failing to recommend/offer an elective caesarean section in the presence of known risk factors for vaginal delivery
- Failing to identify and advise that delivery should be expedited by caesarean section after labour has commenced when there are signs of fetal distress.
Newborn babies can suffer a number of complications that can damage their developing brain if not promptly diagnosed and treated.
The most common complications that give rise to claims of clinical negligence include:
- Failing to diagnose and/or treat neonatal infection, such as group B streptococcus infection which can lead to meningitis and brain injury.
- Failing to diagnose and/or appropriately treat hypoglycaemia (low blood sugar). Some babies have particular risk factors for hypoglycaemia, such as prematurity or babies born to a mother who had diabetes during pregnancy, and therefore require more careful monitoring. Other babies may not have risk factors, but may show recognised signs of hypoglycaemia requiring further investigation and prompt treatment.
- Failing to diagnose and/or appropriately treat jaundice (hyperbilirubinemia). Some babies have particular risk factors for jaundice, such as being born before 38 weeks gestation, or a sibling who suffered jaundice requiring treatment. These babies would require more careful monitoring following their birth. Other babies may not have risk factors, but may show recognised signs of jaundice that require further investigation and treatment. Failing to diagnose and/or treat jaundice in a newborn baby can lead to the baby suffering kernicterus, which is a particular type of damage to the brain leading to cerebral palsy and hearing loss.
An umbilical cord prolapse is when the umbilical cord (which transfers oxygen and nutrients from the placenta to the baby) descends through the opening of the womb before the baby does. In turn, the cord becomes trapped when the baby is being delivered, depriving the baby of oxygen and potentially causing brain damage or death.
Because of the risks to the baby, umbilical cord prolapse is an obstetric emergency and the baby should be delivered by emergency caesarean section.
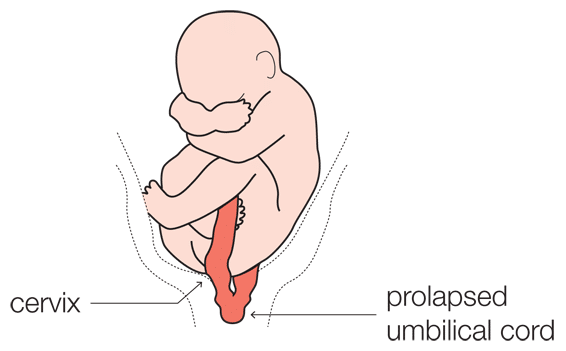
If there are risk factors for cord prolapse, i.e. a baby in the transverse position, then the waters should be broken under controlled conditions. The operating theatre should be prepared to perform an emergency caesarean section should the cord prolapse.
Examples of negligence relating to the management of umbilical cord prolapse include:
- Failing to diagnose, or late diagnosis, of umbilical cord prolapse
- Delay in delivering the baby following diagnosis of umbilical cord prolapse
- Failing to relieve the pressure on the umbilical cord by applying pressure to the presenting part of the baby
- Failing to place the mother on her left side during anaesthetic procedures.
If the baby is in a position to be delivered bottom first, instead of head first, it’s in the breech position. There are additional risks associated with delivering a breech baby vaginally, including an increased risk of oxygen deprivation that can cause brain damage and cerebral palsy if not managed correctly.
If a breech presentation is diagnosed during pregnancy, and the baby’s position does not subsequently change, then there should be a discussion with the mother about the risks and benefits of a caesarean section versus a vaginal delivery. If there are significant risk factors associated with a vaginal delivery, the mother should be advised to have a caesarean section.
If the breech presentation is not diagnosed during pregnancy or labour, the mother might proceed with a vaginal delivery without knowledge of the risks involved.
Examples of negligence relating to the management of a breech presentation include:
- Failing to advise the mother of the options for delivery, including the risks and benefits of all options, following diagnosis of a breech presentation
- Failing to carry out appropriate examinations during pregnancy and/or labour to appropriately diagnose the position of the baby, and therefore failing to diagnose breech presentation
- Failing to act on signs of distress during an attempted breech vaginal delivery.
Shoulder dystocia is an obstetric emergency where the shoulder of the baby becomes impacted (stuck) against the mother’s pelvis during vaginal delivery following delivery of the baby’s head. If the baby’s shoulder is not released swiftly then the baby will be deprived of oxygen. This can cause brain damage leading to cerebral palsy.
Allegations of negligence can be made if there is a failure to carry out appropriate steps in response to a shoulder dystocia that could lead to a delay in the delivery and the baby being deprived of oxygen.
A baby/child/adult may also have grounds for pursuing a claim in the event of suffering injury as a result of shoulder dystocia during their birth, where their mother had known risk factors for shoulder dystocia, but was not informed of these or given the option of an elective caesarean before proceeding with a vaginal delivery which she would have opted for.
You can find out more about shoulder dystocia in our Erb’s palsy section.
If a baby has suffered brain damage due to a lack of oxygen (hypoxic-ischemia), then the umbilical cord blood results will be examined to try to establish the likely timing of this damage, e.g. whether it happened immediately before delivery or some time before.
In order to function normally, the body has to stay at a constant pH (pH figures are used to specify the acidity or basicity (alkalinity) of a solution). The body achieves this by maintaining a healthy balance between chemical acids and chemical bases.
Most of the energy in the body is produced from a chemical reaction that turns sugar (glucose) and oxygen into carbon dioxide and water. This process is called aerobic respiration. When the body is deprived of oxygen it can create energy by an alternative reaction that turns glucose to lactic acid. This process is called anaerobic respiration.
Both lactic acid and carbon dioxide are chemical acids. A build-up of these chemicals results in the blood becoming acidic (acidosis). Oxygen and glucose are transported around the body in the blood. In the womb a baby receives oxygen- and glucose-rich blood from the mother via the umbilical vein. The umbilical artery carries carbon dioxide and other waste products away.
After birth, blood will usually be taken from the umbilical cord to measure the pH value of the blood from the umbilical artery and the umbilical vein. The results will also illustrate the level of carbon dioxide in the blood and the base deficit. The base deficit represents the amount of chemical base that would need to be added to the acidic blood to turn it back to a neutral pH. All of this information can provide valuable clues to the condition of the baby just before and during delivery.
For example, if a cord prolapse occurs during delivery and becomes compressed, the flow of oxygen-rich blood to the baby – and the flow of carbon dioxide and other waste products away from the baby – would be disrupted, causing a build-up of carbon dioxide. To compensate, the baby will start making energy from anaerobic respiration, resulting in the build-up of lactic acid. As the level of carbon dioxide and lactic acid builds up, the pH drops and the amount of chemical base needed to neutralize the acid or base deficit increases.
- Normal umbilical arterial blood will have a pH of between 7.18 and 7.38 and a base deficit of between -8 to 0
- Normal umbilical venous blood will have a pH of between 7.25 and 7.45 and a base deficit of between -8 to 0.
If the damaging period of oxygen deprivation occurred immediately prior to birth, then the umbilical cord blood results will usually show a low pH (typically less than 7) and a base deficit of greater than -12. This is relevant when arguing that delivery should have taken place earlier to avoid injury.
If the umbilical cord blood gas analysis does not show any evidence of acidosis, it may indicate that the damage did not occur immediately prior to delivery.
The results will also be compared with blood taken from the baby shortly after delivery.
Large-scale studies of children and adults with cerebral palsy in the US indicate two key factors that influence life expectancy – their mobility and ability to feed.
People with cerebral palsy who are able to walk unaided, or roll/sit, generally have longer life expectancy than those who have very limited mobility. This is because those with limited mobility are generally weaker, and will find it harder to fight illness and infection. They are also more dependent on the care of others to help prevent life-threatening illnesses and accidents.
People with feeding problems, such as difficulty chewing and swallowing, are more susceptible to choking and aspiration. This increases the risk of life-threatening conditions such as pneumonia. If their condition is more severe, they will be dependent on others for preventing choking and also for their nutrition.
It therefore follows that the quality of care provided to those with cerebral palsy is also a relevant factor in life expectancy.
Other factors affecting life expectancy for people with cerebral palsy include epilepsy, weight management and respiratory conditions.
Statistics can only ever be a guide and factors affecting how long someone will live for vary.
Parents of children with cerebral palsy and those suffering cerebral palsy are naturally interested in their life expectancy; and if you’re pursuing a clinical negligence claim, an estimate of life expectancy is necessary to calculate the compensation for lifetime needs.
The generally accepted starting point for estimating life expectancy is to consider American research and statistics:
- Strauss DJ, Shavelle RM, Rosenbloom L, Brooks JC (2008). Life expectancy in cerebral palsy: An update. Developmental Medicine & Child Neurology, 50:487-493
- Brooks JC, Strauss DJ, Shavelle RM, Tran LM, Rosenbloom L, Wu YW (2014). Recent trends in cerebral palsy survival. Part II: individual survival prognosis. Developmental Medicine & Child Neurology, 56:1065-1071
This research estimates life expectancy for those with cerebral palsy at ages 15, 30, 45 and 60 based on the person’s mobility and feeding ability.
In respect of mobility, the different categories of abilities are:
- Cannot lift head
- Lifts head or chest
- Rolls/sits
- Walks unaided.
In respect of feeding, the different categories of abilities are:
- Tube-fed
- Fed by others
- Self-feeding (further defined as self-feeding for at least 10% of the time).
In order to estimate life expectancy, the statistics in the Strauss tables are adopted for the appropriate abilities, and at the closest age.
For example, a 15-year-old female with cerebral palsy who is self-feeding, but cannot walk unaided, would have an estimated life expectancy of 49 years from age 15 (age 63). This is compared with the life expectancy for the general population, which is an estimated 66 years from age 15 (age 81).
Statistics based on mobility and feeding can then be adjusted for other factors, such as epilepsy.
The Strauss statistics relate to the US population. There are no equivalent statistics available for people with cerebral palsy in the UK and general life expectancy statistics vary between the US and UK (the life expectancy in the UK is higher than in the US).
So how do we apply US research for the purpose of calculating the costs of future lifetime needs in a clinical negligence claim for cerebral palsy in the UK?
The accepted method is to compare, as a percentage, the two estimated life expectancies provided in the American studies and then apply this percentage to the relevant UK life expectancy statistics, published by the Office of National Statistics.
For example:
- A 15-year-old American girl with cerebral palsy who feeds herself, but cannot walk unaided, has an estimated life expectancy of a further 49 years versus a further 65.8 years estimated for the general population.
- She will, therefore, reach 74.5% of the life expectancy estimated for someone the same age without cerebral palsy.
- We apply 74.5% to the life expectancy of a 15-year-old girl in England and Wales (as published by the UK Office of National Statistics) to obtain the estimated life expectancy for a 15-year-old girl with cerebral palsy who feeds herself, but cannot walk unaided.
Cerebral palsy compensation
How is it calculated and how much are you likely to receive?
When your claim for birth injury is successful, it is a lawyer’s job to ensure that the correct level of compensation is paid in order to meet your child’s needs for the rest of their life. These calculations are very complicated.
In the event of an injury, your lawyer will seek compensation to pay for:
Care
It is likely that your child will require some degree of care for the rest of their life. Your lawyer will calculate both past, present and future care costs. A care expert will assess the past care already provided by the parents, the level of care required currently and determine whether these needs are likely to increase in the future. Future care costs are usually calculated on the basis of a commercial care team.
From this, the expert will put together a costed plan. This may include daytime carers, night-time carers, and/or case managers to coordinate care plans.
Accommodation
It is highly likely that you will need to move to a new house which will need to be adapted to meet the needs of your child. Lawyers, with the assistance of an architectural expert, will calculate how much this will cost alongside the ongoing costs involved with maintenance.
Therapies
It is likely that your child requires a number of therapies, which they struggle to access on the NHS such as physiotherapy, occupational therapy, or speech and language therapy. We will include the costs of all therapies required on a private paying basis, as part of the claim for birth injury.
Loss of earnings
Your child’s brain injury may mean that they are unable to work in any capacity in the future, or that they are limited in their choice of work. Lawyers will consider what losses arise from the inability to earn any or a higher wage, as a result of the injury.
Equipment and Transport
It is likely that your child will need specialist equipment throughout their life, for example, a powered wheelchair, or as they get older special hoists to get them in and out of the bath. The initial costs, the maintenance costs and the replacement costs for these items will all be costed.
Likely compensation amounts for cerebral palsy
The way that damages are calculated means that no two cases are the same and any financial losses you and/your child may incur will have to also be taken into account, however the Judicial Guidelines for compensation can give you a good guide to how much you or your child might receive in general damages (damages for pain, suffering and loss of enjoyment of life) in a cerebral palsy claim.
The total value of a cerebral palsy claim is likely to be between £15 to £25 million depending on the severity of the injury, where the family live and the level of care required. Each case will be individually assessed to ensure the maximum compensation levels are claimed.
-
£247,280 to £354,260
Your child may be able to follow basic commands, open their eyes and return to sleep and waking patterns, and have some postural reflex movement. However, they will demonstrate little meaningful response to their environment and little to no language function. They will also have double incontinence and need full-time care.
The top bracket will be appropriate for a child only when there is a significant effect on their senses and they are severely limited physically, e.g. ‘locked in’ syndrome. They will also have substantially restricted life expectancy, e.g. under 15 years.
The amount will be affected by:
- the degree of insight, if any;
- life expectancy;
- the extent of physical limitations;
- requirement for gastronomy for feeding;
- sensory impairment;
- ability to communicate with or without assistive technology;
- extent of any behavioural problems.
-
£192,090 to £247,280
Your child will be very seriously disabled and dependant on others for their care, both professional and otherwise.
They may have physical disabilities such as limb paralysis, or cognitive disabilities with marked impairment of intellect and personality.
Any risks of further developmental issues will also have an effect on the value of the claim, alongside:
- the degree of insight, if any;
- life expectancy;
- the extent of physical limitations and potential for future deterioration;
- the degree of dependence on others;
- ability to communicate;
- extent of any behavioural problems;
- epilepsy or a significant risk of
- epilepsy (unless a provisional damages order provides for this risk).
-
£131,620 to £192,090
Your child has moderate to severe intellectual deficit, a personality change, problems with their sight, speech and senses, and is at significant risk of epilepsy with no prospect of employment.
-
£79,530 to £131,620
Your child has moderate to modest intellectual deficit, their ability to work is greatly reduced if there at all, and they are at risk of developing epilepsy.
-
£37,760 to £79,530
Your child has trouble with concentration and memory, their ability to work is reduced, and they have a small risk of epilepsy. Their dependence on others is limited.
These compensation amounts are strictly guidelines for general damages only and do not represent the total value of the claim, which could be settled for much more than above depending on your child’s personal circumstances. However, as mentioned above, our solicitors will work to secure the maximum level of compensation for your child to ensure their needs are looked after for life.
How can you ensure that a child’s compensation will meet their needs for the rest their life?
Compensation for a child brain injury is usually awarded by way of a lump sum, and an annual periodical payment which is index-linked in line with inflation. This goes to ensure that your child has enough money to last the rest of their life.
As mentioned, payments are ‘index-linked’. This means that even if the cost of employing carers or some other expense increases significantly, your child’s annual payments will rise in order to meet that cost. This gives many parents peace of mind, to know that their children’s care and other requirements will be met in the event that they’re no longer able to care for their child themselves.
Where your child will lack capacity on reaching adulthood, the Court of Protection will appoint a professional Deputy to manage the child’s financial affairs going forward.
Our dedicated Court of Protection team, who have a number of experienced Deputies, is able to assist with financial management and protection of funds throughout your child’s lifetime, giving you peace of mind for the future.

Finding answers
If you want to find out more about your how your child’s cerebral palsy was caused, you’re in the right place. Our team of specialist birth injury solicitors have years of experience finding answers when a child has suffered brain damage at birth.
If you want to find out more about making a claim for compensation, or how we can help to manage your child’s finances, please click here.
We also have guidance on the process of seeking answers through the Early Notification Scheme and Healthcare Safety Investigation Branch (HSIB), which is usually the first port of call if your child has cerebral palsy as a result of a birth injury.


















